(Alzheimer’s Association) The Alzheimer’s Association and the Alzheimer’s Impact Movement (AIM), the Association’s advocacy arm, celebrate the passage of the bipartisan Recognize, Assist, Include, Support, and Engage (RAISE) Family Caregivers Act. Signed into law this week by the president, the RAISE Family Caregivers Act will address the needs of our nation’s family caregivers through the development and implementation of a coordinated national strategy.
The Alzheimer’s Association and the Alzheimer’s Impact Movement (AIM), the Association’s advocacy arm, are celebrating the passage of the bipartisan Recognize, Assist, Include, Support, and Engage (RAISE) Family Caregivers Act.
Signed into law today by the president, the RAISE Family Caregivers Act will address the needs of our nation’s family caregivers through the development and implementation of a coordinated national strategy.
Introduced in Congress by Senators Susan Collins (R-Maine) and Tammy Baldwin (D-Wis.) and Representatives Gregg Harper (R-Miss.) and Kathy Castor (D-Fla.), the RAISE Family Caregivers Act will provide much needed support to family caregivers. The new law directs the Department of Health and Human Services (HHS) to develop a national strategy to provide education and training, long-term services and supports, and financial stability and security for caregivers.
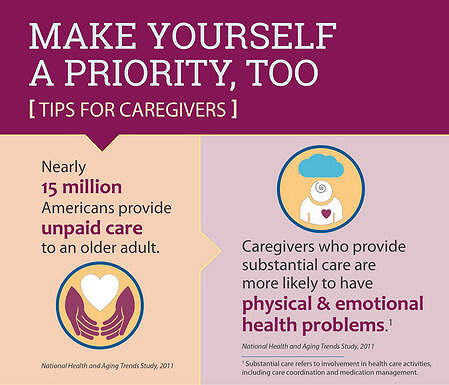
“On behalf of the more than 15 million Americans who provide unpaid care for people living with Alzheimer’s and dementia, we want to thank Sens. Collins and Baldwin, and Reps. Harper and Castor for their bipartisan support for family caregivers,” said Robert Egge, Alzheimer’s Association Chief Public Policy Officer and AIM Executive Director.
“The development of a national strategy will have an immense impact on family caregivers. Enhancing assistance for family caregivers will result in improved caregiver health and well-being and will result in a higher quality of care for their loved ones.”
For millions of Americans caring for individuals with Alzheimer’s and other dementias the emotional, physical and financial costs can be overwhelming. Caregivers of people with dementia report higher levels of stress, depression and worse health outcomes than those providing care to individuals without dementia. As a result, Alzheimer’s caregivers incurred $10.9 billion in additional health costs last year.
The RAISE Family Caregivers Act also directs HHS to create a Family Caregiving Advisory Council, similar to the National Plan to Address Alzheimer’s Disease Advisory Council. Both the advisory council and The RAISE Family Caregivers Act was closely modeled after the National Alzheimer’s Project Act. The Alzheimer’s Association and AIM have been strong advocates for the RAISE Family Caregivers Act since it was introduced in Congress. Grassroots advocates and staff held thousands of congressional meetings to secure support for the legislation. The Association and AIM will continue to play an active role in the process as HHS works to develop and implement the national strategy.
For more information: https://www.govtrack.us/congress/bills/115/s1028
Alzheimer’s Association®
The Alzheimer’s Association is the leading voluntary health organization in Alzheimer’s care, support and research. Our mission is to eliminate Alzheimer’s disease through the advancement of research; to provide and enhance care and support for all affected; and to reduce the risk of dementia through the promotion of brain health. Our vision is a world without Alzheimer’s. For more information, visit alz.org.
Alzheimer’s Impact Movement
The Alzheimer’s Impact Movement (AIM) is a nonpartisan, nonprofit advocacy organization working in strategic partnership with the Alzheimer’s Association. AIM advocates for policies to overcome Alzheimer’s disease, including increased investment in research, improved care and support, and development of approaches to reduce the risk of developing dementia. For more information, visit alzimpact.org

Copyright © 2018 Alzheimer’s Association®. All rights reserved.