Dear Readers,
At year end, a lot of online news services provide a retrospective of the top Alzheimer’s news for 2015. I combed through many articles and found one written by , a journalist at MedicalNewsToday.com. He did a great job of summarizing where we are today with AD causes, symptoms, treatments, and research. If you are interested in a comprehensive overview, read on.
~ Jennifer
(MedicalNewsToday) Alzheimer’s disease is a neurological disorder in which the death of brain cells causes memory loss and cognitive decline. A neurodegenerative type of dementia, the disease starts mild and gets progressively worse.
Fast Facts on Alzheimer’s Disease
Here are some key points about Alzheimer’s. More detail and supporting information is in the main article.
- Alzheimer’s disease is the most common type of dementia. The term “dementia” describes a loss of mental ability associated with gradual death of brain cells.
- There are an estimated 5.3 million Americans of all ages with Alzheimer’s disease.
- An estimated 5.1 million people are age 65 and older, and approximately 200,000 individuals are under the age of 65.
- Every 67 seconds someone in the US develops the disease.
- It is the only cause of death in the US top 10 that cannot be prevented, cured or slowed.
- Almost two thirds of Americans with Alzheimer’s disease are women.
- 1 in 3 seniors dies with Alzheimer’s or another dementia.
- Alzheimer’s and other dementias cost the nation $226 billion per year.
- Due to the physical and emotional toll of caregiving, Alzheimer’s and dementia caregivers had $9.7 billion in additional health care costs of their own in 2014.
- As the population of the United States ages, Alzheimer’s is becoming a more common cause of death.
Causes of Alzheimer’s Disease
Like all types of dementia, Alzheimer’s is caused by brain cell death. It is a neurodegenerative disease, which means there is progressive brain cell death that happens over a course of time.
The total brain size shrinks with Alzheimer’s - the tissue has progressively fewer nerve cells and connections.
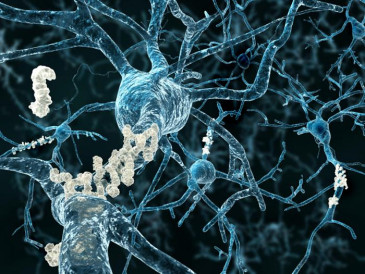 Nerve cells (neurons) in the brain. In Alzheimer’s, there are microscopic ‘plaques’ and ‘tangles’ between and within brain cells.
Nerve cells (neurons) in the brain. In Alzheimer’s, there are microscopic ‘plaques’ and ‘tangles’ between and within brain cells.
While they cannot be seen or tested in the living brain affected by Alzheimer’s disease, postmortem/autopsy will always show tiny inclusions in the nerve tissue, called plaques and tangles:
- Plaques are found between the dying cells in the brain - from the build-up of a protein called beta-amyloid (you may hear the term “amyloid plaques”).
- The tangles are within the brain neurons - from a disintegration of another protein, called tau.
For a detailed visualization of what goes on in the Alzheimer’s disease process, progressing from the normal brain to increasing dementia changes, the Alzheimer’s Association has produced a journey of 16 slides. See the illustrations: Inside the brain: an interactive tour.
The abnormal protein clumps, inclusions, in the brain tissue are always present with the disease, but there could be another underlying process that is actually causing the Alzheimer’s - scientists are not yet sure.
This sort of change in brain nerves is also witnessed in other disorders, and researchers want to find out more than just that there are protein abnormalities - they also want to know how these develop so that a cure or prevention might be discovered.
Symptoms of Alzheimer’s Disease
The information in this section connects closely to some of that about tests and diagnosis below because symptoms noticed by patients, or people close to them, are exactly the same signs that healthcare professionals look for during testing.
Symptoms can be diagnosed at any stage of Alzheimer’s dementia and the progression through the stages of the disease is monitored after an initial diagnosis, too, when the developing symptoms dictate how care is managed.
Of course, the very nature of the symptoms can be confusing for both a patient and the people around them, with different levels of severity. For this reason, and because symptoms could signal any of a number of diagnoses, it is always worthwhile seeing a doctor.
For doctors to make an initial diagnosis of Alzheimer’s disease, they must first be satisfied that there is dementia - guidelines spell out what dementia consists of. It involves cognitive or behavioral symptoms that show a decline from previous levels of “functioning and performing” and interfere with ability “to function at work or at usual activities.”
The cognitive decline is in at least TWO of the five symptom areas listed below (from guidelines jointly produced by the National Institute on Aging and the Alzheimer’s Association):
1. Worsened ability to take in and remember new information, for example:
- Repetitive questions or conversations
- Misplacing personal belongings
- Forgetting events or appointments
- Getting lost on a familiar route.
2. Impairments to reasoning, complex tasking, exercising judgment:
- Poor understanding of safety risks
- Inability to manage finances
- Poor decision-making ability
- Inability to plan complex or sequential activities.
3. Impaired visuospatial abilities (but not, for example, due to eye sight problems):
- Inability to recognize faces or common objects or to find objects in direct view
- Inability to operate simple implements, or orient clothing to the body.
4. Impaired speaking, reading and writing:
- Difficulty thinking of common words while speaking, hesitations
- Speech, spelling, and writing errors.
5. Changes in personality and behavior, for example:
- Out-of-character mood changes, including agitation; less interest, motivation or initiative; apathy; social withdrawal
- Loss of empathy
- Compulsive, obsessive or socially unacceptable behavior.
Once the number and severity of these example symptoms confirm dementia, the best certainty that they are because of Alzheimer’s disease is given by:
- A gradual onset “over months to years” rather than hours or days (the case with some other problems)
- A marked worsening of the individual person’s normal level of cognition in particular areas.
The most common presentation marking Alzheimer’s dementia is where symptoms of memory loss are the most prominent, especially in the area of learning and recalling new information. But the initial presentation can also be one of mainly language problems, in which case the greatest symptom is struggling to find the right words.
If visuospatial deficits are most prominent, meanwhile, these would include inability to recognize objects and faces, to comprehend separate parts of a scene at once (simultanagnosia), and a type of difficulty with reading text (alexia). Finally, the most prominent deficits in “executive dysfunction” would be to do with reasoning, judgment and problem-solving.
Stages of Alzheimer’s Disease
The progression of Alzheimer’s can be broken down into three basic stages:
- Preclinical (no signs or symptoms yet)
- Mild cognitive impairment
- Dementia.
The Alzheimer’s Association has broken this down further, describing seven stages along a continuum of cognitive decline based on symptom severity - from a state of no impairment, through mild and moderate decline, and eventually reaching “very severe decline.”
The association has published the seven stages online. It is not usually until stage four that a diagnosis is clear - here it is called mild or early-stage Alzheimer’s disease, and “a careful medical interview should be able to detect clear-cut symptoms in several areas.”
How Common is Alzheimer’s Disease?
In the US, the most recent census has enabled researchers to giveestimates of how many people have Alzheimer’s disease. In 2010, some 4.7 million people of 65 years of age and older were living with Alzheimer’s disease in the US.
The 2013 statistical report from the Alzheimer’s Association gives a proportion of the population affected - just over a tenth of people in the over-65 age group have the disease in the US. In the over-85s, the proportion goes up to about a third.
As our dementia page outlines, there is a handful of different types, but Alzheimer’s disease is the problem behind most cases of memory loss and cognitive decline:
The Alzheimer’s Association says it accounts for between 60% and 80% of all cases of dementia.
Vascular dementia, which is caused by stroke not Alzheimer’s, is the second most common type of dementia.
Alzheimer’s Disease Risk Factors
Some things are more commonly associated with Alzheimer’s disease - not seen so often in people without the disorder. These factors may therefore have some direct connection. Some are preventable or modifiable factors (for example, reducing the risk of diabetes or heart disease may in turn cut the risk of dementia).
If researchers gain more understanding of the risk factors, or scientifically prove any “cause” relationships for Alzheimer’s, this could help to find ways to prevent it or develop treatments.
Risk factors associated with Alzheimer’s disease include:
Unavoidable risk factors
- Age - the disorder is more likely in older people, and a greater proportion of over-85-year-olds have it than of over-65s.
- Family history (inheritance of genes) - having Alzheimer’s in the family is associated with higher risk. This is the second biggest risk factor after age.
- Having a certain gene (the apolipoprotein E or APOE gene) puts a person, depending on their specific genetics, at three to eight times more risk than a person without the gene. Numerous other genes have been found to be associated with Alzheimer’s disease, even recently (see developments below).
Potentially avoidable or modifiable factors
- Factors that increase blood vessel (vascular) risk - including diabetes, high cholesterol and high blood pressure. (These also increase the risk of stroke, which itself can lead to another type of dementia.)
- Low educational and occupational attainment.
- Prior head injury. (While a traumatic brain injury does not necessarily lead to Alzheimer’s, some research links have been drawn, with increasing risk tied to the severity of trauma history.)
- Sleep disorders (the breathing problem sleep apnea, for example).
Early-onset Alzheimer’s disease
Genetics are behind early-onset familial Alzheimer’s disease, which presents typically between the ages of 30 and 60 years and affects people who have a family history of it.
Due to one of three inherited genes, it is also known as young-onset, and it is uncommon - accounting for under 5% of all Alzheimer’s cases.
The Alzheimer’s Association says in its early-onset information that it can sometimes be “a long and frustrating process” to get this diagnosis confirmed since doctors do not expect to find Alzheimer’s in younger people. For the younger age groups, doctors will look for other dementia causes first.
Healthcare professionals, the nonprofit says, may also “incorrectly attribute” symptoms to stress and so on, or may not agree on the diagnosis.
Recent developments in understanding causes and risk factors from MNT news
Could high blood sugar be a cause of Alzheimer’s disease?
While nobody knows exactly what causes the complex brain changes that lead to Alzheimer’s disease, scientists suspect one of the drivers is the accumulation of plaques of a faulty protein called beta-amyloid. Now, a new study of mice shows how too much sugar in the blood can speed up the production of the protein.
New mechanism behind Alzheimer’s onset identified
A new study published in the journal Brain overturns thinking on the role of toxic peptides in the development of Alzheimer’s disease.
Could sleeping on one’s side reduce risk of Alzheimer’s?
Although the findings are yet to be tested in humans, a study suggests sleeping posture affects how well the brain clears away waste products. Accumulation of waste products in the brain is a hallmark of neurodegenerative diseases such as Alzheimer’s and Parkinson’s.
Fat deposits in brain may hasten Alzheimer’s disease
A breakthrough in Alzheimer’s research reveals that an abnormal build-up of fat droplets in the brain may cause or speed up the disease. The finding promises to open new avenues in the search for a cure or new treatments.
Could Alzheimer’s be transmitted through medical procedures?
A medical procedure involving injections of a discontinued human growth hormone has been linked to the transmission of a protein associated with Alzheimer’s disease in a number of patients, according to a new study published in the journalNature.
Study sheds light on how stress may raise risk of Alzheimer’s
Previous research has linked stress with increased risk of Alzheimer’s disease, but the mechanisms underlying this association have been unclear. Now, researchers from the University of Florida believe they are one step closer to an explanation.
Tests and Diagnosis for Alzheimer’s Disease
Alzheimer’s disease is not simple to diagnose - there is no single test for it. For this reason, the first thing doctors do is to rule out other problems before confirming whether mental signs and symptoms are severe enough to be a kind of dementia or something else.
Doctors may:
- Take a history (ask about symptoms and daily activities)
- Do a physical examination to find any signs of, for example, a stroke, heart condition or kidney disease, and
- Check neurological function, e.g. by testing balance, senses and reflexes.
Depending on what the doctor thinks could need checking, other diagnostics are:
- Sending off for tests of blood and urine samples
- Arranging brain scans (possibly including CT, MRI and EEG).
Sometimes dementia symptoms are related to an inherited disorder such as Huntington’s disease, so genetic testing may be done. For some, an assessment for things such as depression can also be carried out.
Again though, the above early tests are not for diagnosing Alzheimer’s disease itself, but for ruling out other problems before starting to narrow down to dementia caused by AD. Central to this is checking memory loss and mental performance (cognitive testing).
There must be memory loss and an impairment in one other area of cognition for a diagnosis of dementia such as Alzheimer’s to be made. These criteria also need to be progressive (a worsening compared with how the person has been before), and severe enough to affect daily activities.
Because of this common route to a diagnosis for all kinds of dementia, there is more detailed information about this from theMedical News Today dementia page; the following summary also gives links straight to particular sections on that page.
Cognitive tests have changed little since being established by work from the likes of Professor Henry Hodkinson in the 1970s. The following example list of questions reveals the types of memory loss and areas of cognition that are tested and may indicate Alzheimer’s.
The “abbreviated mental test score” (AMTS):
- What is your age?
- What is the time, to the nearest hour?
- Repeat an address at the end of the test that I will give you now (e.g. “42 West Street”)
- What is the year?
- What is the name of the hospital or town we are in?
- Can you recognize two people (e.g. the doctor, nurse, home help, etc.)?
- What is your date of birth?
- In what year did World War 1 begin? (Other widely known dates in the past can be used.)
- Name the president/prime minister/monarch.
- Count backwards from 20 down to 1.
The general practitioner assessment of cognition (GPCOG) test is a website-based assessment designed to be an early reliable indicator for use in initial consultations with GPs.
The mini mental state examination (MMSE) is a fuller cognitive test to help diagnose Alzheimer’s disease. It is also sensitive to the severity of the disorder and helps to indicate when drug treatment could ease symptoms appearing later in the course of the disease:
- Normal cognitive health - score above 26
- Mild-to-moderate Alzheimer’s - below 26
- Moderate - below 20 but above 10
- Severe - score under 10.
It is always worthwhile for people with concerns about their own or someone else’s possible dementia to get the problem thoroughly checked by a doctor, both because of the mental confusion created by the symptoms and because they may be due to something else that needs checking and treating.
Is there a biological test for Alzheimer’s disease?
There is no simple biological test specifically for Alzheimer’s disease that can be used by doctors, which is why all the diagnostic options are designed to rule out other explanations for the dementia before confirming Alzheimer’s as the cause.
A genetic test is possible in some settings to indicate the likelihood of someone having or developing the disease but this is controversial and not entirely reliable. A gene known as the APOE-e4 is associated with higher chances of people over the age of 55 years developing Alzheimer’s.
The question of future biological tests is being intensely investigated by medical research. A lot of clues as to the biological changes in the brain have been uncovered by neuropathology work on brains examined at autopsy after death. This and other types of research may result in future tests to measure new biomarkers.
Genetic testing may become a more realistic option, too - so long as researchers continue to find reliable links as they discover new gene associations.
Genetic testing is not always a welcome idea though. The Alzheimer’s Association’s position on APOE-e4 testing for example, is that it should not be used routinely and that there should not be prejudiced treatment in terms of insurance and so on when it is used as an indication.
In research studies, any genetic results used as indicators of disease would not be identifiable by individual - they would be anonymized.
Recent developments in tests and diagnosis from MNT news
Peanut butter may help diagnose Alzheimer’s disease
A small study published in August 2013 in the Journal of the Neurological Sciences found interesting differences in ability to smell peanut butter between people with Alzheimer’s disease versus those with different kinds of dementia.
Could a simple saliva test detect Alzheimer’s?
A person’s risk of Alzheimer’s disease could be predicted through a simple saliva test, according to the results of a new study.
New way of looking at age could help prevent Alzheimer’s
A team of researchers at King’s College London in the UK has announced the development of a “gene signature” that could help predict conditions such as Alzheimer’s disease years before symptoms arise.
Changes in humor may be early indicator for dementia
According to new research, a noticeable change in what makes us laugh may not be a good sign for cognitive health: it may be an early indicator for dementia.
Treatment and Prevention of Alzheimer’s Disease
There is no known cure for Alzheimer’s disease - the death of brain cells in the dementia cannot be halted or reversed.
There is, however, much backing for therapeutic interventions to help people live with Alzheimer’s disease more ably.
The Alzheimer’s Association includes the following as important elements of dementia care:
- Effective management of any conditions occurring alongside the Alzheimer’s
- Activities and/or programs of adult day care
- Support groups and services.
America has created a national plan to address Alzheimer’s disease, making it a medical priority for the country.
In January 2011, President Obama signed the National Alzheimer’s Project Act into law, stating:
“Alzheimer’s disease burdens an increasing number of our nation’s elders and their families, and it is essential that we confront the challenge it poses to our public health.”
Along with an aim to improve research into prevention and treatment, the goals of the plan also include measures for present interventions:
- Enhance care quality and efficiency
- Expand supports for people with Alzheimer’s disease and their families, and
- Enhance public awareness and engagement.
Drug therapy
There are no disease-modifying drugs available for Alzheimer’s disease but some options may reduce its symptoms and help improve quality of life. There are four drugs in a class called cholinesterase inhibitor approved for symptomatic relief in the US:
- Donepezil (brand name Aricept)
- Alantamine (Reminyl)
- Rivastigmine (Exelon)
- Tacrine (Cognex).
A different kind of drug, memantine (Namenda), an NMDA receptor antagonist, may also be used, alone or in combination with a cholinesterase inhibitor.
Other therapy
As with other types of dementia and neurodegenerative disease, a major part of therapy for patients with Alzheimer’s comes from the support given by healthcare workers to provide dementia quality-of-life care, which becomes more important as needs increase with declining independence.
Recent developments in treatment and prevention from MNT news
Drug successfully reverses effects of Alzheimer’s in rats
A new study indicates that a drug may represent a novel therapeutic target for Alzheimer’s disease after researchers used it to treat the disease in rats.
Red wine compound found to stabilize Alzheimer’s biomarker
A clinical trial assessing the compound resveratrol in people with mild to moderate Alzheimer’s disease has revealed that it stabilizes a biomarker found to decline alongside the progression of the disease.
Existing arthritis drug bodes well for Alzheimer’s
An existing prescription drug may be able to help in the fight against Alzheimer’s, according to research published inNature Medicine.
New Alzheimer’s treatments may arise from modeling ‘heat shock proteins’
One of the hallmarks of Alzheimer’s disease is the abnormal clumping of beta-amyloid proteins in the brain, resulting in the death of brain cells. The discovery that small heat shock proteins prevent uncontrolled protein clumping has opened the possibility of developing drugs that emulate this effect. Now, a new study takes this a step further by revealing how small heat shock proteins interact with beta-amyloid to prevent clumping.
Antibody test could detect Alzheimer’s at preventable stage
An antibody test that can accurately detect the presence of Alzheimer’s disease before symptoms appear may soon be available, according to researchers from the Rowan University School of Osteopathic Medicine. It would give physicians an opportunity to intervene at the earliest, most treatable stage.
Alzheimer’s: newly identified molecular mechanism could lead to treatment
During the early stages of Alzheimer’s disease, when individuals appear to be free of symptoms, toxic changes are nevertheless taking place in the brain - including synapse loss. Though scientists do not yet fully know what causes this form of dementia, researchers have found how brain cell connections are destroyed in early stages of the disease.
Prevention
There is a lot of research into risk factors associated with Alzheimer’s disease, so there may be lifestyle measures we can take to potentially reduce our risk and enjoy a healthier life more generally. Medical News Today has a page compiling ideas from researchers on how to prevent Alzheimer’s disease and dementia - including information about heart health, diet, exercise and keeping an active brain.
More Information
Some of the information about Alzheimer’s disease also applies to other types of cognitive decline. See our broader page about dementia - you will also find links to useful parts of that page in some of the sections about Alzheimer’s below.

http://www.medicalnewstoday.com/articles/159442.php#risk_factors
Written by Markus MacGill
Last updated: Friday 4 December 2015
MacGill, M. (2015, December 4). “Alzheimer’s Disease: Causes, Symptoms and Treatments.” Medical News Today. Retrieved from http://www.medicalnewstoday.com/articles/159442.php.